Genetic factors
Type 2 diabetes develops largely as a result of genetic factors. Numerous facets of our health, including how our bodies process glucose and react to the hormone insulin, which
controls blood sugar levels, are influenced by our DNA.Certain gene variants may increase the risk of developing type 2 diabetes. The general operation of cells involved in the synthesis of insulin, insulin sensitivity, and glucose metabolism can be impacted by these genetic alterations. A person may be more prone to type 2 diabetes if they acquire these gene variations from their parents.
Family history also plays an important role in understanding genetic factors. Your chance of getting type 2 diabetes rises if a close relative—such as a parent or sibling—has the disease.This increases the likelihood that the illness can be inherited.Genetic factors interact with other risk factors, such as obesity, a sedentary lifestyle, and poor dietary choices, to influence the development of type 2 diabetes.
For example, individuals with certain gene variants may be more prone to develop insulin resistance, a condition in which the body’s cells become less responsive to the effects of insulin. This can lead to high blood sugar levels and eventually lead to type 2 diabetes.
Obesity and sedentary lifestyle
Obesity: Carrying too much body weight, especially in the abdomen, raises the possibility of getting type 2 diabetes. When a person is overweight or obese, the body’s cells become less sensitive to insulin, making it harder for insulin to effectively regulate blood sugar levels. Over time, insulin resistance can lead to high blood sugar levels and type 2 diabetes.
Obesity is often the result of a combination of genetic, lifestyle and environmental factors.Consuming foods and drinks that are high in calories, bad fats, and sugar can make you gain weight.Conversely, a sedentary lifestyle promotes weight gain and insulin resistance. The body’s capacity to appropriately manage blood sugar is diminished by prolonged sitting or light exercise.Type 2 diabetes risk is increased as a result.
Poor diet and nutrition
Poor diet and nutrition are major contributing factors in the development of type 2 diabetes. When individuals constantly eat unhealthy foods and lack proper nutrition, it can lead to weight gain, insulin resistance, and elevated blood sugar levels. Let’s find out how a poor diet affects the risk of type 2 diabetes:
1) A diet high in processed and refined foods, such as sugary snacks, fast food and packaged foods, significantly increases the risk of type 2 diabetes. These foods often contain high amounts of added sugars, unhealthy fats, and refined carbohydrates. Consuming too much of these ingredients can lead to weight gain, insulin resistance, and elevated blood sugar levels.
2) Regular consumption of sugary drinks, including soda, sweetened juices and energy drinks, is strongly associated with an increased risk of developing type 2 diabetes.
3) Foods rich in unhealthy fats, such as saturated fats and trans fats, contribute to the development of type 2 diabetes. These fats are commonly found in fried foods, processed snacks, and high-fat dairy products. Eating too much of these fats can lead to obesity, insulin resistance, and imbalances in blood lipid levels.
Consume a variety of fruits and vegetables to get essential vitamins, minerals and dietary fiber. Choose whole grains over refined grains to ensure a steady release of glucose into the bloodstream. Avoid sugary drinks and opt for water, unsweetened tea or coffee. Limiting foods high in saturated fat and trans fat, such as fried foods, pastries and processed snacks.
Diuretic
A diuretic is a type of medication that is commonly used to increase urine production and encourage the excretion of excess fluid from the body. These drugs work by affecting the kidneys, specifically the tubules responsible for reabsorbing water and electrolytes. They help reduce fluid retention and blood pressure by increasing the amount of urine produced and eliminating excess fluid from the body.
There are different types of diuretics, including:
1) For high blood pressure, Thiazide diuretics are frequently recommended. They work by inhibiting the reabsorption of sodium and chloride in the kidneys, thereby increasing urine production. Thiazide diuretics help relax blood vessels, reduce the workload of the heart, and lower blood pressure.
2) Loop diuretics are often used for conditions such as congestive heart failure and edema. They act on the loop of Henle, a segment of the kidney tubule, and inhibit the reabsorption of sodium, chloride, and water.
3) Potassium-sparing diuretics help promote urine production by retaining potassium, an essential electrolyte. These diuretics work by blocking the effects of aldosterone, a hormone that promotes sodium and water reabsorption in exchange for potassium excretion.It is important to note that diuretics can have side effects and should be used under the guidance of a healthcare professional. Common side effects include increased urination, electrolyte imbalance, dehydration, and changes in blood pressure.
Metabolic syndrome
The chance of developing cardiovascular disease, type 2 diabetes, and other health issues rises when a group of disorders known as metabolic syndrome co-occurs. It is characterized by a combination of factors including obesity, high blood pressure, high blood sugar levels, abnormal cholesterol levels and increased waist circumference. To be diagnosed with metabolic syndrome,
a person must have at least three of the following criteria:
1) Accumulation of excess fat around the waist, often indicated by an increase in waist circumference. In men, a waist circumference of 40 inches or more and for women, a measurement of 35 inches or more is indicative of central obesity.
2) High blood pressure equal to or greater than 130/85 mmHg, or taking high blood pressure medication.
3) Fasting blood glucose levels equal to or greater than 100 mg/dL (5.6 mmol/L), or previously diagnosed with type 2 diabetes.
4) Insulin resistance occurs when cells in the body become less responsive to the effects of insulin, resulting in high levels of insulin in the blood. Metabolic syndrome is influenced by several factors, including genetics, obesity, physical inactivity, poor diet, and aging.
For those with metabolic syndrome,
some suggestions are as follows:
1) Losing weight, especially around the waist, can improve insulin sensitivity and reduce the risk of complications.
2) It is important to eat a balanced diet that is low in saturated fat, trans fat and refined carbohydrates. Place a focus on lean protein, healthy fats, fruits, vegetables, whole grains, and cereals.
3) Regular physical activity, such as aerobic exercise and strength training, can improve insulin sensitivity, lower blood pressure and help with weight loss.
4) Medicines may be needed to control high blood pressure or abnormal cholesterol levels. Regular monitoring and adherence to prescribed treatment is essential.
5) For people with diabetes proper management of blood sugar levels through medication, diet and lifestyle changes is crucial. Regular blood sugar monitoring and medical guidance are required.
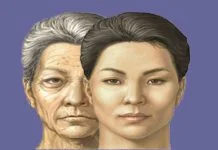
Age and race
Age and race are two important factors that affect the risk of developing certain health conditions, including type 2 diabetes. Let’s delve into each of these factors extensively:Age: Increasing age is a significant risk factor for type 2 diabetes. The risk of developing this condition increases as individuals age. This is partly due to age-related changes in the body, including a decrease in insulin sensitivity and a decrease in the function of the beta cells in the pancreas, which produce insulin.It is important to note that age alone does not cause type 2 diabetes.
The more risk factors and normal aging processes a person is exposed to, the more likely they are to develop the condition.Race and ethnicity can also affect the risk of developing type 2 diabetes. Some racial and ethnic groups are more prone to the condition than others.
For example:-African Americans have a higher risk of developing type 2 diabetes than some other ethnic groups. They are more likely to develop the condition at a younger age and experience more severe complications.Hispanic/Latino Americans, especially those of Mexican or Puerto Rican descent, have a higher risk of type 2 diabetes than non-Hispanic whites. Additionally, they typically start showing symptoms younger.
Native Americans, including Native Alaskans and Native Hawaiians, have a significantly higher risk of developing type 2 diabetes than other racial and ethnic groups.Certain subgroups of Asian Americans, such as South Asians and Filipinos, have a higher risk of type 2 diabetes than other Asian American subgroups.The increased risk of type 2 diabetes among these racial and ethnic groups can be attributed to a combination of genetic, lifestyle, and socioeconomic factors.
Gestational diabetes
A form of diabetes that develops during pregnancy. It is characterized by high blood sugar levels that are first detected during pregnancy in women. Gestational diabetes usually occurs between the 24th and 28th week of pregnancy and usually resolves after delivery. It is important that having gestational diabetes increases the risk of developing type 2 diabetes later in life.
During pregnancy, the body undergoes hormonal changes that can affect how insulin hormone that regulates blood sugar, is produced and used. Gestational diabetes occurs when the body cannot produce enough insulin to adequately control blood sugar levels during pregnancy.
Risk factors for gestational diabetes include:
1) Women who become pregnant over the age of 35, have a higher risk of developing gestational diabetes.
2) A family history of diabetes increases the risk of gestational diabetes.
3) Women who have had gestational diabetes in a previous pregnancy are more likely to develop it in a subsequent pregnancy.
4) Before becoming pregnant, overweight or obese raises the risk of gestational diabetes.
5) PCOS is a hormonal disorder that can increase the risk of gestational diabetes.
Controlling gestational diabetes is crucial for the health of mother and baby. If left uncontrolled, that can cause complications during pregnancy and delivery. After birth It can also increase the baby’s risk of health problems.
Treatment of gestational diabetes usually:
1) Regular monitoring of blood sugar levels helps ensure that they are within target range.
2) Following a balanced diet recommended by dietitian is essential. These include choosing nutrient-dense foods, controlling carbohydrate intake, and spreading meals and snacks.
3) Engaging in regular physical activity helps control blood sugar levels and improve overall health during pregnancy.
4) In some cases, insulin injections needed to control blood sugar levels.
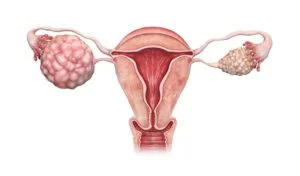
Polycystic Ovary Syndrome (PCOS)
Hormonal condition known as polycystic ovarian syndrome affects women who are of reproductive age. It is characterized by a combination of symptoms related to hormonal imbalance, ovarian dysfunction and metabolic abnormalities. PCOS is a complex condition that can have various manifestations and effects on a woman’s health.
Let’s explore PCOS :
1) Women with PCOS experience imbalances in hormone levels, especially androgens and insulin. This imbalance can disrupt the normal functioning of the ovaries, leading to ovulation difficulties and the development of small ovarian cysts.
2) PCOS often causes menstrual irregularities. Irregular periods, prolonged periods or missing periods. Hormonal imbalances and ovulatory dysfunction can affect the regular release of eggs from the ovaries, resulting in irregular periods.
3) The ovaries of people with PCOS frequently have tiny, fluid-filled cysts. These cysts are usually harmless and do not require specific treatment.
4) Many women with PCOS also experience insulin resistance. Their bodies have trouble using insulin efficiently.
5) PCOS can present with a variety of symptoms and effects. These can include excessive hair growth on the face, chest or back, acne, hair loss, difficulty gaining or losing weight, darkening of the skin and mood swings.
6) PCOS is a common cause of infertility due to disruption of ovulation. Women with PCOS may experience difficulty conceiving and may require medical interventions such as fertility drugs or assisted reproductive technology to achieve pregnancy.The precise cause of PCOS is still not entirely understood. There is no cure for PCOS.
Its symptoms can be managed through several methods:
1) Adopting a healthy lifestyle including regular exercise and a balanced diet can help manage PCOS symptoms.
2) Depending on specific symptoms and goals, doctors prescribe medications to help regulate menstrual cycles, reduce excessive hair growth, improve insulin sensitivity.
Medicines and medical terms
Medicines and medical terms play an important role in healthcare by providing treatment for various conditions and facilitating effective communication between healthcare professionals and patients.
Let’s explore these aspects:
1) Medicines also known as pharmaceuticals. This substances used to diagnose, treat, manage or prevent medical conditions. They can be available in different forms like tablets, capsules, injections, creams or inhalers. Healthcare professionals prescribe medications based on diagnosis, symptoms, and individual patient characteristics. Different classes of drugs exist, each designed to target specific symptoms.
Examples:
Antibiotics: Medicines used to treat bacterial infections by killing bacteria.
Analgesics: Medicines that relieve pain, such as opioids.
Antidepressants: Medicines used to treat depression related mental health conditions.
Antihypertensives: Medications prescribed to lower high blood pressure and manage cardiovascular health.
Antidiabetic drugs: used to manage diabetes and control blood sugar levels.
Anticoagulants: Medicines that prevent blood clotting and reduce the risk of thrombosis or stroke.
It is important to follow doctor’s instructions regarding medication dosage, frequency, and possible side effects. Patients should also inform their doctor’s of any allergies, existing medical conditions, or other medications they are taking to avoid adverse interactions.
In Medical Terminology specialized phrases that healthcare professionals use to describe diseases, conditions, symptoms, procedures, and anatomical structures. They provide a standard language for communication in the medical field. Understanding common medical terms is essential for effective communication between healthcare professionals and patients.
Examples:
Diagnosis: Identification of a disease based on symptoms, medical history, and diagnostic tests.
Symptoms: A subjective indication of a disease experienced by the patient, like pain, fever.
Procedure: A medical surgical technique performed to diagnose, treat a condition.
Anatomy: The study of the structure and organization of the human body, including organs, tissues, and systems.
Radiology: Medical specialty that uses imaging techniques, like X-rays, MRIs, or CT scans, to diagnose and treat disease.
Stress and mental health
Stress and mental health are interrelated aspects of our well-being. Stress is the body’s response to demanding or challenging situations.
Let’s explore the relationship between stress and mental health:
1) Understanding Stress is a natural and automatic response of the body to a perceived threat. It can be induced by an array of factors. Like, work-related issues, financial problems, relationship difficulties or major life events. Stress can manifest in both physical and emotional symptoms.
2) Chronic stress can have significant effects on mental health. It can contribute to the development or exacerbation of various mental health conditions, including anxiety disorders, depression, post-traumatic stress disorder (PTSD) and substance abuse disorders.
3) Chronic stress activates the body’s stress response system, releasing stress hormones such as cortisol and adrenaline into the bloodstream.
4) Stress and mental health have a cyclical relationship. Mental health conditions, anxiety or depression, can make individuals more susceptible to experiencing stress.Effective coping mechanisms are essential for managing stress and maintaining good mental
health. Healthy coping strategies may include:
1) Regular physical activity, maintaining a balanced diet and ensuring adequate sleep can reduce stress and support mental well-being.
2) Practicing relaxation techniques, such as deep breathing exercises, meditation can promote relaxation and reduce stress levels.
3) When stress becomes overwhelming seeking help from a mental health professional a therapist or counselor, can provide guidance and support.
4) Prioritizing self-care activities that promote mental well-being is crucial. Taking regular breaks, engaging in hobbies and building positive relationships can contribute to emotional resilience and stress management.
sleep problems
Sleep problems refer to any difficulty in normal sleep patterns that can affect the quantity and quality of a person’s sleep. Sleep is essential to overall health and well-being. Sleep problems can have a significant impact on physical, mental, and emotional functioning. Let’s explore this topic:
Sleep problems can manifest in a number of ways, including:
1) Difficulty falling asleep, staying asleep, or experiencing unrefreshing sleep.
2) Sleep apnea: interrupted breathing during sleep, poor sleep quality, and daytime fatigue.
3) A neurological disorder characterized by excessive daytime sleepiness, sudden sleep attacks, and sleep-wake cycles.
4) Abnormal behaviors during sleep, such as sleepwalking, nightmares, or night terrors.
Sleep problems can have many causes, including:
1) High levels of stress or worry might make it challenging to unwind and go to sleep.
2) Certain medical conditions, such as chronic pain, hormonal imbalances, can cause sleep disturbances.
3) Unhealthy sleeping habits, irregular sleep schedules, excessive alcohol consumption, and exposure to electronic devices before bedtime can contribute to sleep problems.
4) Noise, uncomfortable bedding, too much light can interfere with sleep.
Sleep problems can significantly affect many aspects of life:
1) Poor sleep can lead to excessive daytime sleepiness, loss of concentration, and impaired cognitive function.
2) Sleep problems are associated with increased risk of mood disorders such as depression and anxiety.
3) Inadequate sleep can weaken the immune system, making individuals more susceptible to illness and infection.
Effective management of sleep problems may include:
1) Establishing a regular sleep schedule, creating a comfortable sleep environment.
2) Techniques such as cognitive-behavioral therapy for insomnia can help address underlying causes and improve sleep quality.
3) In some cases, medication or medical intervention may be needed to manage sleep problems.
Conclusion
Understanding the factors that contribute to type 2 diabetes is crucial for prevention, management, and overall wellness. Several key factors have been identified, including genetic factors, obesity and sedentary lifestyle, poor diet and nutrition, diuretic use, age and race, gestational diabetes, and metabolic syndrome. Some medications, such as diuretics, can affect blood sugar control.
It is important to work closely with healthcare professionals and monitor blood sugar levels regularly when taking diuretics or any other medication that may affect diabetes management.diabetes type 2 is a complex condition influenced by a combination of genetic, lifestyle and environmental factors. Byunderstanding these factors and taking proactive steps to address them, individuals can reduce their risk of developing type 2 diabetes and manage the condition effectively if already diagnosed.